Fibromyalgia is a chronic pain disorder that affects millions of people worldwide, yet its exact causes remain misunderstood and often misdiagnosed. If you’ve been struggling with persistent pain, extreme fatigue, brain fog, and sleep disturbances, you’re not alone. Fibromyalgia can make even the simplest daily tasks feel overwhelming, leaving many people frustrated and searching for answers.
Despite its complexity, researchers have identified several underlying factors that contribute to fibromyalgia. From nervous system dysfunction and hormonal imbalances to sleep disorders and chronic inflammation, multiple biological and environmental factors may interact to trigger fibromyalgia symptoms. Understanding these root causes is the first step in finding relief and managing this condition effectively.
In this article, we will explore 10 root causes of fibromyalgia that you need to know. By the end, you’ll have a clearer picture of what might be contributing to your symptoms—and, more importantly, what you can do to start feeling better.
Find calm and serenity every day discover how NuviaLab Relax can help reduce stress naturally
What You’ll Learn in This Article:
✅ The connection between fibromyalgia and nervous system dysfunction
✅ How poor sleep quality and stress worsen symptoms
✅ The role of hormones, inflammation, and gut health in fibromyalgia
✅ How lifestyle changes and medical treatments can help you regain control
1. Nervous System Dysfunction (A Key Cause of Fibromyalgia)
Nervous system dysfunction plays a crucial role in the development and persistence of fibromyalgia. Understanding how the nervous system interacts with pain perception can shed light on why individuals with fibromyalgia experience chronic pain, fatigue, and other symptoms.
How the Central Nervous System Increases Pain Sensitivity
- Role of Neurotransmitters Like Serotonin and Norepinephrine:
Neurotransmitters are chemical messengers that transmit signals in the brain and throughout the body. In fibromyalgia, the balance of neurotransmitters, particularly serotonin and norepinephrine, can be disrupted. Serotonin is known to help regulate mood and pain perception, while norepinephrine plays a role in the body’s response to stress and pain modulation. When levels of these neurotransmitters are low, individuals may experience heightened pain sensitivity and emotional disturbances, exacerbating fibromyalgia symptoms. - How Fibromyalgia Leads to an Overactive Pain Response:
In fibromyalgia, the central nervous system becomes hypersensitive to pain signals, a phenomenon known as central sensitization. This means that the brain and spinal cord amplify signals from the body, resulting in a lower pain threshold. Everyday sensations that would normally be considered mild or non-painful can be perceived as intense pain. This overactive pain response can lead to a cycle of pain, where even minimal stimuli trigger significant discomfort, making daily activities challenging.
The Link Between Fibromyalgia and Chronic Stress
- How Long-Term Stress Disrupts the Nervous System:
Chronic stress is another significant contributor to nervous system dysfunction in fibromyalgia. When the body is under continuous stress, it enters a state of hyperarousal, which can disrupt normal brain function and pain processing. The persistent activation of the fight-or-flight response can lead to changes in the way the brain perceives pain, making it more difficult to manage and reducing overall resilience to stress. - The Impact of High Cortisol Levels on Pain and Fatigue:
Cortisol, the body’s primary stress hormone, is released in response to stress. In individuals with fibromyalgia, elevated cortisol levels can lead to increased inflammation and altered pain responses. Prolonged exposure to high cortisol can contribute to symptoms of fatigue, anxiety, and depression, further complicating the fibromyalgia experience. Elevated cortisol can also disrupt sleep patterns, leading to a cycle of fatigue and increased pain sensitivity, creating a vicious cycle that can be difficult to break.
Understanding the role of nervous system dysfunction in fibromyalgia is vital for developing effective management strategies. By addressing these underlying issues, individuals may find relief from symptoms and improve their overall quality of life.
Find calm and serenity every day discover how NuviaLab Relax can help reduce stress naturally
2. The Role of Sleep Disorders in Fibromyalgia Causes
Sleep disorders are commonly associated with fibromyalgia and can significantly impact the severity of symptoms. Understanding the relationship between sleep and fibromyalgia is essential for managing this condition effectively.
Why Poor Sleep Increases Fibromyalgia Symptoms
- Connection Between Sleep Deprivation and Heightened Pain:
Sleep deprivation has been shown to amplify the perception of pain in individuals with fibromyalgia. When the body doesn’t get enough restorative sleep, it can lead to increased levels of substance P, a neurotransmitter that plays a key role in pain processing. Additionally, lack of sleep can lower pain thresholds, making even minor discomfort feel more intense. This heightened sensitivity can result in a cycle of pain and fatigue, further complicating symptom management. - Common Sleep Disorders in Fibromyalgia (Insomnia, Sleep Apnea):
Many individuals with fibromyalgia experience specific sleep disorders, such as insomnia and sleep apnea. Insomnia is characterized by difficulty falling asleep or staying asleep, leading to chronic fatigue and irritability. Sleep apnea, on the other hand, causes interruptions in breathing during sleep, resulting in poor sleep quality and excessive daytime sleepiness. Both disorders can exacerbate fibromyalgia symptoms, making it crucial to identify and address any underlying sleep issues.
How to Improve Sleep to Reduce Fibromyalgia Symptoms
- Tips for Better Sleep Hygiene:
Implementing good sleep hygiene practices can help improve the quality of sleep for individuals with fibromyalgia. Some effective tips include:
- Establish a Regular Sleep Schedule: Go to bed and wake up at the same time every day, even on weekends, to regulate your body’s internal clock.
- Create a Relaxing Bedtime Routine: Engage in calming activities before bed, such as reading, listening to soothing music, or practicing gentle stretches to signal to your body that it’s time to wind down.
- Limit Screen Time Before Bed: The blue light emitted by screens can interfere with the production of melatonin, a hormone that regulates sleep. Aim to avoid screens for at least an hour before bedtime.
- Make Your Sleep Environment Comfortable: Ensure your bedroom is dark, quiet, and cool, and invest in a comfortable mattress and pillows to promote restful sleep.
- The Role of Melatonin and Relaxation Techniques:
Melatonin is a hormone that helps regulate sleep-wake cycles. For some individuals with fibromyalgia, taking melatonin supplements may improve sleep quality and reduce insomnia symptoms. Additionally, incorporating relaxation techniques, such as deep breathing exercises, meditation, or yoga, can help reduce anxiety and promote a sense of calm, making it easier to fall asleep and stay asleep.
Improving sleep quality is a critical component of managing fibromyalgia. By addressing sleep disorders and implementing effective strategies, individuals can experience a reduction in symptoms and an overall improvement in their quality of life.
3. Inflammation and Gut Health: Hidden Triggers of Fibromyalgia
Emerging research highlights the critical role that inflammation and gut health play in fibromyalgia. Understanding these connections can provide insight into the underlying mechanisms of the condition and offer potential avenues for symptom relief.
The Gut-Brain Connection in Fibromyalgia
- How Gut Microbiome Imbalances Contribute to Inflammation:
The gut microbiome, a complex community of microorganisms residing in the digestive tract, has a profound impact on overall health, including the immune system and inflammation. Imbalances in the gut microbiome—often referred to as dysbiosis—can lead to increased intestinal permeability, sometimes referred to as “leaky gut.” This condition allows toxins and inflammatory molecules to enter the bloodstream, triggering an immune response that can exacerbate fibromyalgia symptoms. Research suggests that a healthy gut microbiome is essential for maintaining proper immune function and reducing inflammation. - Link Between Fibromyalgia and Irritable Bowel Syndrome (IBS):
Many individuals with fibromyalgia also report symptoms of Irritable Bowel Syndrome (IBS), a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. The connection between fibromyalgia and IBS may stem from shared underlying factors, such as nervous system dysfunction and chronic inflammation. This overlap suggests that managing gut health and addressing IBS symptoms may help alleviate some fibromyalgia-related discomfort.
Chronic Inflammation and Fibromyalgia Flare-Ups
- The Role of Autoimmune Responses in Worsening Symptoms:
Chronic inflammation is a hallmark of many autoimmune conditions, and some researchers believe that fibromyalgia may involve similar immune system dysregulation. An autoimmune response can lead to persistent inflammation, causing muscle pain, fatigue, and other symptoms associated with fibromyalgia. When the immune system mistakenly targets healthy tissue, it can trigger flare-ups and exacerbate existing pain. - Anti-Inflammatory Diets and Their Potential Benefits:
Adopting an anti-inflammatory diet may offer potential benefits for individuals with fibromyalgia. Such diets typically emphasize whole foods, including fruits, vegetables, whole grains, healthy fats, and lean proteins, while reducing processed foods, sugars, and trans fats. Foods rich in omega-3 fatty acids, such as fatty fish, walnuts, and flaxseeds, may help reduce inflammation and support overall health. Additionally, some studies suggest that specific dietary approaches, such as the Mediterranean diet or gluten-free diets, may improve symptoms for some individuals. Working with a healthcare provider or nutritionist can help tailor dietary changes to individual needs and preferences.
Understanding the intricate relationship between inflammation, gut health, and fibromyalgia is vital for developing effective treatment strategies. By addressing these hidden triggers, individuals may find pathways to relieve symptoms and improve their overall well-being.
4. 10 Root Causes of Fibromyalgia: Hormonal Imbalances and Fibromyalgia Causes
Hormonal imbalances are significant contributors to the complexity of fibromyalgia, influencing pain perception, mood, and overall health. Understanding these imbalances can provide insight into effective management strategies for those affected by this chronic condition.
How Low Serotonin and Dopamine Affect Pain Perception
- The Impact of Neurotransmitter Deficiencies on Mood and Pain:
Neurotransmitters such as serotonin and dopamine play crucial roles in regulating mood and pain perception. Low levels of serotonin are often associated with increased pain sensitivity and can contribute to a cycle of pain and emotional distress. Similarly, dopamine, which is involved in the brain’s reward system, influences feelings of pleasure and motivation. Deficiencies in these neurotransmitters can lead to heightened pain perception, making it difficult for individuals with fibromyalgia to cope with their symptoms effectively. - Why People with Fibromyalgia Often Experience Depression and Anxiety:
The interplay between hormonal imbalances and emotional health is particularly evident in fibromyalgia. Many individuals with this condition experience depression and anxiety, which can be exacerbated by low levels of serotonin and dopamine. The constant struggle with chronic pain can lead to feelings of hopelessness, further impacting mood and increasing the likelihood of developing anxiety disorders. Recognizing and addressing these emotional components is essential for comprehensive fibromyalgia management.
The Connection Between Thyroid Disorders and Fibromyalgia
- How Hypothyroidism Can Mimic Fibromyalgia Symptoms:
Thyroid disorders, particularly hypothyroidism, can present symptoms that overlap significantly with fibromyalgia, such as fatigue, muscle weakness, and joint pain. An underactive thyroid can lead to metabolic slowdowns, causing a range of symptoms that may confuse diagnosis and treatment. For individuals with both fibromyalgia and hypothyroidism, distinguishing between the two conditions is crucial for effective management. - The Role of Hormonal Therapy in Symptom Management:
For those diagnosed with hypothyroidism, hormonal therapy—typically in the form of thyroid hormone replacement—can alleviate symptoms and improve overall quality of life. By restoring normal hormone levels, individuals may experience increased energy, reduced fatigue, and better pain management. For those with fibromyalgia, addressing hormonal imbalances through various therapies, including medications and lifestyle changes, may also contribute to symptom relief and improved well-being.
Understanding the role of hormonal imbalances in fibromyalgia is vital for developing effective treatment plans. By addressing these underlying issues, individuals can find more targeted approaches to manage their symptoms and enhance their overall quality of life.
5. Environmental & Lifestyle Factors That Trigger Fibromyalgia
Environmental and lifestyle factors play a critical role in triggering and exacerbating fibromyalgia symptoms. Understanding these influences can empower individuals to make informed choices that may alleviate their condition.
The Impact of Toxins and Heavy Metals on Fibromyalgia
- How Mold Exposure, Pollution, and Chemicals Can Trigger Symptoms:
Exposure to environmental toxins, such as mold, heavy metals, and pollutants, has been linked to the onset and exacerbation of fibromyalgia symptoms. Mold exposure can lead to chronic inflammatory responses, affecting the immune system and potentially contributing to increased pain and fatigue. Additionally, chemicals found in everyday products, including cleaning supplies and pesticides, can disrupt hormonal balance and impact overall health. Heavy metals, like lead and mercury, can accumulate in the body and may lead to neurological impairments, further aggravating fibromyalgia symptoms. - Detox Strategies to Reduce Environmental Stressors:
Implementing detox strategies can help reduce the burden of environmental toxins. Some effective approaches include:
- Creating a Clean Living Environment: Regularly clean and ventilate living spaces to reduce mold and dust accumulation. Consider using air purifiers to improve indoor air quality.
- Choosing Natural Products: Opt for non-toxic cleaning and personal care products to limit exposure to harmful chemicals.
- Incorporating Nutrient-Rich Foods: A diet rich in antioxidants, vitamins, and minerals can support the body’s detoxification processes. Foods like leafy greens, berries, and cruciferous vegetables are excellent choices.

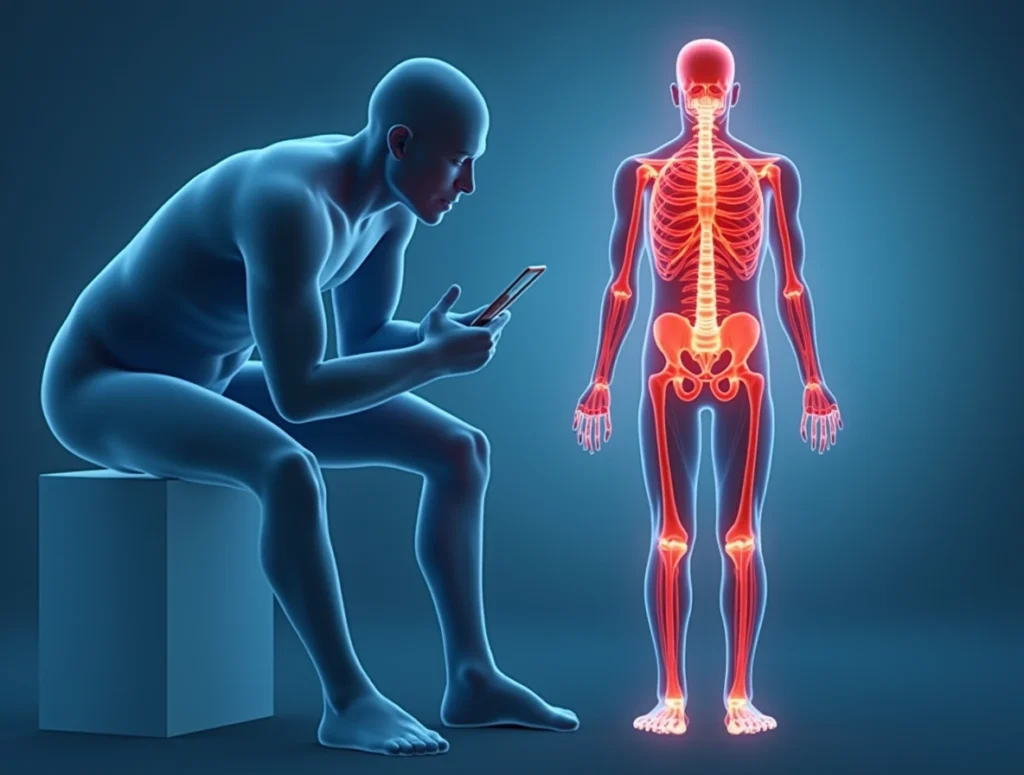
Why a Sedentary Lifestyle Worsens Fibromyalgia Symptoms
- The Importance of Regular Movement for Managing Pain:
A sedentary lifestyle can significantly worsen fibromyalgia symptoms by contributing to muscle stiffness, decreased strength, and increased pain sensitivity. Regular movement helps maintain muscle flexibility and strength, which is essential for managing pain and improving overall function. Engaging in physical activity releases endorphins, the body’s natural painkillers, providing a sense of relief from fibromyalgia symptoms. - Gentle Exercises Like Yoga and Stretching for Relief:
Incorporating gentle exercises, such as yoga and stretching, can be particularly beneficial for individuals with fibromyalgia. These activities promote relaxation, improve flexibility, and enhance circulation, which can help alleviate pain and reduce stress. Mindfulness practices, such as deep breathing and meditation, can further enhance the benefits of yoga by promoting mental well-being. Additionally, walking and low-impact aerobic exercises can provide a safe way to incorporate movement into daily routines without exacerbating symptoms.
Recognizing and addressing environmental and lifestyle factors that contribute to fibromyalgia is crucial for effective symptom management. By making informed choices and prioritizing movement, individuals can take proactive steps toward improving their overall health and quality of life.
Conclusion
Fibromyalgia is a complex and often misunderstood condition that can significantly impact the lives of those who suffer from it. Understanding the ten root causes of fibromyalgia is crucial for effective management and relief of symptoms. Factors such as nervous system dysfunction, sleep disorders, inflammation, hormonal imbalances, and environmental triggers all play a role in the onset and exacerbation of this condition.
By recognizing how these factors interact, individuals can take proactive steps toward managing their symptoms through lifestyle changes, dietary adjustments, and seeking appropriate medical care. It’s essential to adopt a holistic approach that includes physical activity, stress management techniques, and emotional support to improve overall well-being.
If you or someone you know is struggling with fibromyalgia, remember that you’re not alone. Connecting with healthcare professionals, support groups, and resources can provide valuable assistance and empower you on the journey toward better health. Together, we can raise awareness about fibromyalgia and foster a supportive community for those affected by this challenging condition.
Frequently Asked Questions (FAQs) About Fibromyalgia
- What is fibromyalgia?
- Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. It affects how the brain processes pain signals, leading to heightened sensitivity to pain.
- What are the common symptoms of fibromyalgia?
- Common symptoms include widespread pain, fatigue, sleep disturbances, difficulty concentrating (often referred to as “fibro fog”), headaches, irritable bowel syndrome (IBS), and mood disorders like anxiety and depression.
- What causes fibromyalgia?
- The exact cause of fibromyalgia is unknown, but it is believed to result from a combination of genetic, environmental, and psychological factors. Common contributing factors include nervous system dysfunction, hormonal imbalances, sleep disorders, and chronic stress.
- How is fibromyalgia diagnosed?
- Fibromyalgia is diagnosed based on a patient’s medical history, reported symptoms, and a physical examination. There are no specific laboratory tests for fibromyalgia, but doctors may rule out other conditions that could cause similar symptoms.
- What treatments are available for fibromyalgia?
- Treatment for fibromyalgia typically includes a combination of medication, physical therapy, lifestyle changes, and alternative therapies. Common medications include pain relievers, antidepressants, and anticonvulsants. Non-pharmacological treatments may include exercise, cognitive-behavioral therapy, and mindfulness techniques.
- Can diet affect fibromyalgia symptoms?
- Yes, diet can play a role in managing fibromyalgia symptoms. Some individuals may find relief by adopting an anti-inflammatory diet, which includes whole foods, fruits, vegetables, lean proteins, and healthy fats while avoiding processed foods, sugar, and excessive caffeine.
- Is fibromyalgia a progressive condition?
- Fibromyalgia is not considered a progressive disease, meaning it does not worsen over time. However, symptoms can vary in intensity and may flare up or improve based on various factors such as stress, activity level, and lifestyle changes.
- Can exercise help with fibromyalgia?
- Yes, regular, low-impact exercise can help reduce fibromyalgia symptoms. Activities such as walking, swimming, yoga, and stretching can improve flexibility, strength, and overall well-being while helping to manage pain.
- Are there any support groups for people with fibromyalgia?
- Yes, many support groups exist for individuals with fibromyalgia, both in-person and online. These groups provide a space for sharing experiences, coping strategies, and emotional support.
- How can family and friends support someone with fibromyalgia?
- Family and friends can support someone with fibromyalgia by being understanding and patient, listening to their experiences, helping them with daily tasks when needed, and encouraging them to seek professional help and engage in activities that promote well-being.


